Dr. Christensen said in Dentistry Today (Feb 2000), “The three major diseases we treat are caries, periodontal disease, and occlusion. Occlusion remains the major untreated disease in dentistry today. We probably treat caries too much, perio a little and we don’t even talk about occlusion.” How does an occlusion age? Or a better question for your patient is: Is your patient’s occlusion ageing at a faster rate than the patient’s age? This lecture takes a closer look at many factors in the lifetime of an occlusion that accelerate the wear and tear on the teeth and the temporomandibular joints. Also included are some clinical symptoms and anatomy changes that develop as the bite ages. Occlusion is a strong topic among dentists. Abfractions have been classified, MRI’s of the Temporomandibular Joints show how a meniscus ages, and muscle trigger patterns have become universally accepted. The paradigm that occlusion and periodontal pockets are not related is disappearing fast. Occlusion is about growth and development, airway, posture and habitual patterns in today’s 3-D digital format. Digital cone beam technology now provides a 3-D image of anatomy.
Dental care, education, and a genetic trend toward healthier teeth, gums and bone have extended human life and the lifetime of the dentition. Each generation saves more teeth and it might be possible for a natural dentition to last 120 years or more in the future. For now, these teeth are producing a new set of trends in our patients at every age group of life. Each decade of life brings a new challenge to the teeth, gums, jaw joints and the muscles that drive their function.
Below are ten trends that are changing in our patients that relate to occlusion:
Many young children (3-8) present with high vaulted palates, deviant swallows, allergies and mouth breathing. Early orthodontic care is the best value in modern dentistry today because it can correct so many growth and development problems.
Age’s 6, 12 and 18 are the best times to check the occlusion of a growing child. Age 6 for airway, Age 12 for asymmetry in the canine region and age 18 for jaw and condyle development.
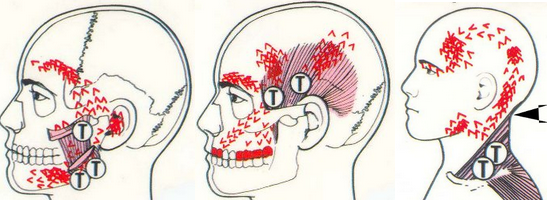
A large number of young female patients (age 20-35) have frequent muscle tension/migraine headaches. Unfortunately, the female T.M. joint can be weak anatomically, as compared to the male. A stressed, stretched, or torn posterior lateral ligament of the T.M. meniscus produces temporal headaches. The female T.M. ligaments can be hyper-mobile at a young age and never tighten. Twenty-year-old patients should not pop their jaw joints. An unstable occlusion at 20 will tear up the joints in the female by age 40.
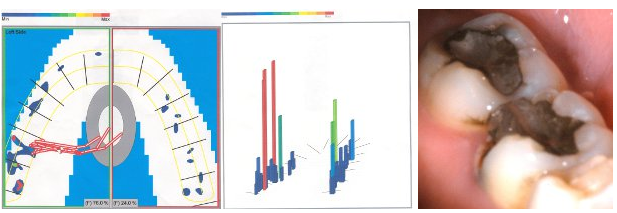
(The T-Scan pattern below is a 30-year-old female with a torn right posterior/lateral ligament of the right meniscus.)
Habitual Force Patterns – One or two unhealthy T.M. joints change the bite quickly. The T-Scan is an instrument that shows how the force that is generated when teeth occlude is distributed. The bite force is recorded when the patient taps their teeth together on a computer sensor. The program records which teeth hit, how hard they contact and in what sequence the teeth work together. When the stomatognathic system functions, a sequence of force that has an origin, direction, and intensity is generated. Mapping and recording the force distribution produces a unique repeatable signature force pattern named the Habitual Force Pattern (HFP). HFP is a diagnostic force map that was captured as the patient swallowed, squeezed and tapped firm on a T-Scan recording sensor. Each HFP movie is a summary of approximately 100 frames of force in sequence, much like MRI sections, showing how the cycle of force is transferred on the occlusion. Force cycles can be both functional and dysfunctional.
This patient has muscle pain and triggers on a daily basis on the right side, and has a 10-year history of right temporal/migraine headaches. The problem with this bite pattern is that all the anterior guidance is on the posterior teeth. This patient loved her bite splint because it turned down the muscle triggers illustrated in the pictures below.
The lingual cusp of a lower molar is almost always the first cusp to fracture in the 20-40 year old patient. Sometimes it’s the upper distal buccal cusp. The jaw joints compress and after a couple of decades of chewing, the T.M. joints can flatten much like a tire with a slow leak. As the joints age the back teeth take more force. This example of a T-Scan force pattern is a 30-yr old female with a left T.M. disorder. The Distal/Lingual cusp on #19 is fractured and the 3-D scan shows her bite squeezed into MIP. The 2-D scan shows a dysfunctional HFP.
- Most baby boomers have many different restorations and materials in their mouth. Sometimes the same arch will have gold, porcelain, silver, composite, and natural teeth. At times, we see crowns only in the lower left and upper right or vice versa. Many patients present with dental materials that are not working together. Different materials wear at different rates and changing dental philosophies can be hard on an occlusion. Adding more materials and more crowns can increase the stress on the occlusion, especially if the existing dentistry is out of alignment.
- Most bicuspid ortho extraction cases of the 1960’s, 70’s and 80’s do not hold. These bites are in trouble 10 years post ortho and many will have destroyed the occlusion only 20 years post ortho. We have known this bite to be a problem for jaw joints for years. In some months, half of my new T.M. disorder patients were once treated as an ortho extraction case. Unstable occlusial planes cause a bite to turn or collapse quickly, much like missing a lower first molar at a young age.
- After treating T.M. disorders for twenty years, 70 percent of all new patients are female, age 25-55. There are many reasons but an interesting note is that T.M. pain goes away during pregnancy, but comes back strong six months after the baby is born. Most of these patients have lived with a popping jaw their entire adult life. During pregnancy, head and neck muscle tension headaches fade away and the chewing muscles are free to adapt how they want. After pregnancy, the unilateral headaches and jaw popping can increase at an accelerated rate, and the individual may be forced to try and find a new muscle engram to chew. Each pregnancy can weaken the temporomandibular joints, teeth and periodontal ligaments, and increase the stress on the occlusion. Females tend to turn on their condyles while men compress the T.M. joints.
- Middle aged men tend to have jaw joints that are so strong that occlusial stress does not go to the T.M. lateral ligaments like the middle aged female. If a man’s jaw is going to compress, then the force will generally go to the teeth and bone. Men will crowd their lower anterior teeth when the occlusion is stressed for years. Both men and women in their 50’s can crowd the lower anteriors and force all the incisal edges of all the anterior teeth to wear uneven and fast. We call this poor anterior guidance, but the problem started decades previous with the posterior teeth, and an off center envelope of function.
- If a jaw joint is compressed for a lifetime or exceeds its’ bio-load capacity, then you will hear crepitus (sand paper sounds) with your stethoscope in any movement of the mandible. My older patient’s aging in their 70’s, 80’s and 90’s, usually have a hearing aide in the same ear as the heavy crepitus. I have no idea if jaw disorders accelerate hearing disorders, but lack of blood supply in the temporal region over the years may be the reason.
- After 15 years experience with implants, their ability to hold an occlusion together can be a small miracle and a key puzzle piece to saving a bite. Implants in the molar region along with a good envelope of function and good anterior guidance can save an occlusion, and over time a pseudo disc will form in the joint capsule, and joint sounds will disappear. Implants can improve muscle efficiency and improve the envelope of function.
The repetitive movement of chewing, swallowing, yawning, and talking produce dynamic muscle engrams that is unique to every individual. The most common example of a habitual muscle engram is your signature. We learn oral muscle engrams at a young age and these patterns may help or hinder the growth and development of the jaw, bite and muscles.
In the young occlusion (age 0-10), the most important factor is heredity and airway. I see a large number of young patients (primary dentition) with high vaulted palates, and airway constriction. At age five a perfect flat upper palate means the nasal airway is wide open and the patient has a neutral swallow. Age eight is an excellent time to check arch development. If the lower arch does not fit center to the upper arch at a young age the child will develop a lifetime of asymmetric muscle patterns. Early orthodontic care has been a very big paradigm shift in recent years and will continue to grow at a rapid rate.
Canines and second molars erupt around age 11, and lock in many of the muscle patterns that we will develop for our lifetime. Young and healthy bites function much like a rabbit and chew in a small tight circle. Older or unhealthy bites function in an over-exaggerated wider envelop of function, which accelerates the wear and tear on the teeth, gums and jaw joints.
Teenagers, who chew gum all day, every day, function in a neutral envelop of function. Other kids who either can’t chew gum or start popping their jaw after chewing gum are probably on their way to accelerating a more stressful chewing cycle. At age 20, the skull, jaw and teeth development is complete. The muscle patterns have been developing an engram pattern for over a decade. After age 20, the adult chewing cycle or what dentists call the envelope of function will often determine how a bite will age over their lifetime.
The third decade of life uncovers the sometimes-subtle periodontal changes of a stressed occlusion. I see a strong relationship between the periodontal ligaments that support the teeth and the posterior lateral ligament of the T.M. meniscus. A poor or stressed occlusion has the teeth and muscles trapped between the joint and teeth ligaments. This is usually the decade of the popping jaw joints, abfractions, perio pockets and muscle tension headaches
If ligaments fail to function or are stressed, stretched or torn, then the muscle must adapt and help the ligaments hold the jaw and teeth tight. Muscles cannot contract for long periods of time without fatigue. They will change the engram and start some of the muscle trigger patterns shown previous. Occlusions can age quickly if the muscle engrams are changing. Ligaments, muscles, teeth, and perio health must all work in harmony to prevent an occlusion from premature ageing.
