Occlusion is just a good centric, and no interferences, and the rest is all hogwash.

- Centric means center and refers to a condyle position.
- Two symmetrically perfect condyles, in a center position, in the same patient is rare so the term centric relation was born.
- Centric relation changes over time, so as the TM joints age the correct term is now Adaptive Centric Posture.
- No matter what the term is called, if the two condyles are healthy enough to center the occlusion at the point of contact then all is good. It does not matter what the back swing (envelope of function) looks like if the club face (mandible) is center to the ball (occlusal contact).
All good occlusions start with two healthy jaw joints, normal muscle activity, normal tensile forces on the teeth/prosthesis, and good oral hygiene. Dr. George Hollenbeck (famous for the Hollenbeck Carver dental instrument) said: “They make too much out of this. Occlusion is just a good centric, and no interferences, and the rest is all hogwash.” The basic goals of centric are simple; however, achieving them can become complicated. As dentists, we relentlessly pursue the mastery of centric throughout our careers!
The word centric means central. In dentistry, centric is a concept that refers to the position of the TMJ condyle heads within the glenoid fossa. The best analogy to think of is that of a pencil in a vertical position supporting an upside down bowl. If the pencil balances the bowl, then the pencil head is in centric. If the pencil is in any other position, forward, backward, either left or right of the center of the bowl, then it will not balance the bowl straight. The glenoid fossa does not have a perfect bowl shape, but you get the idea. A centric position is dictated by the anatomy of each temporomandibular joint. In centric, the ideal anatomical position of the head of the condyle is superior, anterior, and slightly medial within the glenoid fossa, on either side.
The problem in occlusion and centric always comes down to symmetry. Humans have two TM joints and one occlusion (bite), yet very few skulls exhibit symmetrical temporal bones. During craniofacial growth, the two sides of the nasal-maxillary complex are rarely identical. However, the two maxillary bones must be perfectly symmetrical for the sphenoid and temporal bones to be identical in shape and position. Posselt stated that 97% of all bites have a natural CR-CO slide. Why might you ask? If the left temporal fossa does not exactly mirror the right one, the condyle heads will not hold identical positions within their respective glenoid fossa. Usually, the condyle on the ‘good’ airway side will be in centric while the other, on the deviated septum side, will grow slightly out-of-centric. To go back to the bowl and pencil analogy, a pencil on the ‘good’ side would support an upside down bowl while a pencil on the ‘compromised’ side could not balance the bowl.
Nowhere in my text books on occlusion is the word centric defined by itself; however, many authors use phrases like ‘centric closure’ and ‘freedom to centric.’ The term centric can be confusing because it is often juxtaposed to words in expressions which hold radically different meanings such as ‘centric relation,’ ‘centric occlusion,’ ‘long centric,’ ‘habitual centric,’ and ‘myocentric.’ Most dentists, like Dr. Hollenbeck, use centric when referring to centric relation occlusion.
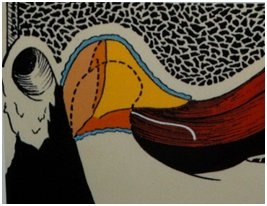
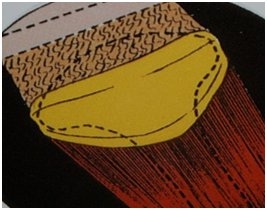
When Dr. Hollenbeck states that “occlusion is just a good centric,” he means that when both TM joints are loaded with force, the condyles are in a physiologically and biomechanically correct position. The orthopedic meaning of centric is based on a closed-pack relationship of the condyle, articular disc, and fossa during function. The closed-pack relationship of articular structures in any joint is considered to be both physiologically and biomechanically correct. A healthy TM joint in centric is illustrated in the two photos below. The first illustration is a lateral view of the TM joint and the second one is a superior view of the meniscus on the head of the condyle.
Joints in the human body such as knees, hips, shoulders, and TMJs, function best when the bones they support are braced, or seated correctly, in all moving positions. When two bones are pressed firmly against the middle of the meniscus, the ligaments that are attached to the meniscus assume a neutral and stable position.
Ligaments are designed to tightly hold a joint and to prevent the bones and meniscus from separating. Ligaments are variably elastic, but they do not function like rubber bands. In general, ligaments in female bodies have more elasticity than those in male bodies, but anatomically, ligaments are not designed to stretch. If the two bones within a joint are not braced tightly against the meniscus in all moving positions, then the ligaments that support the joint become overworked, stretched, or torn. A knee, hip, or jaw joint that is not braced correctly for a million repetitive movements, must adapt. Functional adaptation may be physiologic or pathologic over time, and jaw joints change as occlusion ages.
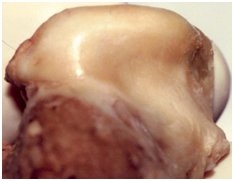
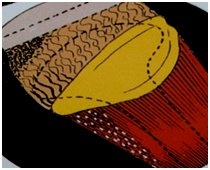
The three illustrations below show how a right condyle stresses first at the lateral pole, how the meniscus starts to change shape, and how the superior head of the lateral pterygoid contracts (white dots). This condyle is no longer in a natural centric relationship during function because it is not 100% ligament-braced in all moving positions. The picture on the right presents a dissected left condyle (the diagrams are of a right condyle) showing how the meniscus is stretched off the lateral pole and bunched up on the medial pole.
TM joints always compress first at the lateral pole of a condyle head. The lateral meniscus ligament attachment fatigues when a condyle translates before rotating completely. Jaw joints stress quickly when asked to translate prematurely. When the posterior lateral meniscus ligament attachment stretches off the lateral pole of a condyle, the meniscus pops on and off the condyle head while active. The superior head of the lateral pterygoid muscle must hold an isometric contraction and protect the damaged or stretched ligament, as shown by the white dots in the middle illustration. The retro distal tissue will stretch and finally tear, changing the blood and the nutrient flow to the TM joint. The anatomical picture shows a right condyle torn on the lateral pole.
As the joint further deteriorates, the patient will lose the ability to hold centric in all functional positions. The degeneration may take months or years to occur. This particular condyle may be painful when stressed, but most condyles in this condition are not. The majority of condyles with a reciprocal click while opening and closing are in this condition. By the time they are 40 years old, half of our patients have at least one condyle in this condition. Dr. Hollenbeck would consider this condyle to be in poor centric and creating an unstable occlusion.
By not being in centric, this condyle in function will start a chain reaction that will age the TM joint at an accelerated rate. Consider this:
- It does not function in a physiologically or biometrically correct position when loaded with chewing force, for example.
- It is not ligament-braced on the lateral pole.
- Its lateral pole is muscle-braced by the superior head of the lateral pterygoid muscle.
- It has lost its ability to rotate correctly so it must translate before the rotation is complete.
- The envelope of function when chewing fades to one side.
- The posterior teeth are under excessive stress on the non-working cusps which promotes tooth fatigue, tooth fracture, and stress on the periodontium.
- The lower anterior incisors are going to wedge causing all incisal edges to wear unevenly because the protrusive slide is off-center.
- Any dentistry performed in centric occlusion on this patient will only accelerate the adaptation of the TM joint over time.
When a natural centric does not exist, a dentist must place the condyles in centric and this position is named adaptive centric posture. The majority of dentists consider centric relation and adaptive centric posture to be identical positions. Both seat the condyle in a joint-ligament dictated position by loading the medial pole and decreasing the stress on the lateral pole.
In dentistry, the adjective centric always refers to the position of the condyles in the glenoid fossa. All expressions formed with the word centric refer to the condyles. For example, centric occlusion refers to the position of the condyles when the teeth are in maximum interlock (MIP). This position is also called acquired centric or habitual centric.
Since condyles are attached to the posterior portion of the mandible, and since the mandible is a single bone, then it must be a physical fact that the adapted position of the condyles in the fossae will be dictated by the dentition. This adaptation may or may not create an ideal condylar-fossa relationship. It could be in a muscularly-braced rather than in a ligamentally-braced position. Many people adapt to such a condition and live with it for years with no trouble. Unfortunately, when under excessive stress, the same people may experience muscle triggers, ligament pain, and degeneration of the stomatognathic system.
If the condyles are in centric relation when all the teeth are in a stable, balanced interlock then the patient is said to be in centric relation occlusion. Dr. L.D. Pankey says in A Philosophy of the Practice of Dentistry, “I see patients who do not have centric relation occlusion within hollering distance.” In dentistry, we have five ways of helping our patients obtain a centric relation occlusion: orthognathics, orthodontics, restoration, splint therapy, and equilibration. The ultimate goal in dentistry is to use the five treatments in a creative yet conservative combination to restore the bite to CRO (centric relation occlusion).
Finally, let’s look at the words myocentric and power centric which refer to a muscle-related position. Neuromuscular dentistry is based on the concept of myocentric occlusion which is obtained by using an electrical neural stimulation to create a neuromuscularly-oriented occlusal position. Myocentric occlusion was defined by Dr. Jankelson as “the terminal point in space at which, with the mandible in rest position, subsequent isotonic muscle contraction raises the mandible through the interocclusal space along the myocentric (muscle-braced) trajectory.”
Occlusion starts with the condyles yet most dentists today practice only in maximum interlock (MIP) and habitual centric. Master dentists of the past advocated that patients should be treated with the goal of establishing a centric relation occlusion, i.e. a “good” centric. For the entire stomatognathic system to function well and with minimal physiological adaptation, the MIP, or habitual centric, in each and every occlusion should match the adaptive centric posture.